🎟️ LifeSource Conference 2025 – 20% Off Sale (Code: Save20) – Deal Ends Sept 15th, 11:59pm CT! Buy now!🎟️
🎟️ LifeSource Conference 2025 – 20% Off Sale (Code: Save20) – Deal Ends Sept 15th, 11:59pm CT! Buy now!🎟️
Heart disease or coronary heart disease (CHD) consists of abnormal functioning of the heart primarily (heart attack, heart failure, arrhythmia, and more). However, in its broader definition it encompasses the bodies vascular system and closely related organs. In this setting it is referred to as cardiovascular disease. Related conditions include cerebrovascular abnormalities (stroke), high blood pressure, peripheral vascular disease (leg pain, amputation), renovascular disease (kidney failure), and more. In this section, we will discuss key components of heart disease and our recommended natural interventions for them.
High blood pressure is a clinical condition in which the systolic blood pressure is persistently greater than 140 mmHg and/or the diastolic blood pressure that is greater than 90 mmHg. It is commonly referred to as Essential Hypertension, the most common form of hypertension. The underlying cause of Essential Hypertension is multifactorial. This form of hypertension may be secondary to vascular abnormalities, hormonal imbalances, renal dysfunction and much more. Underlying abnormalities such as increased oxidative stress, microbiome imbalances or, increased inflammation with or without an autoimmune component. Multiple mechanism are usually involved, making it a more complex disorder to evaluate and treat.
Secondary Hypertension is the other major High Blood Pressure group. It is usually due to a well-defined primary disorder. Examples of primary causes of secondary hypertension include bilateral renal artery stenosis (a vascular abnormality of the kidneys), pheochromocytoma (abnormal hormonal secretion from the adrenal glands), or hyperaldosteronism (abnormal hormonal secretions from the kidneys). Secondary Hypertension is usually successfully treated with treatment of the primary condition.
Hypertension is divided into stages which are outlined in the chart below.
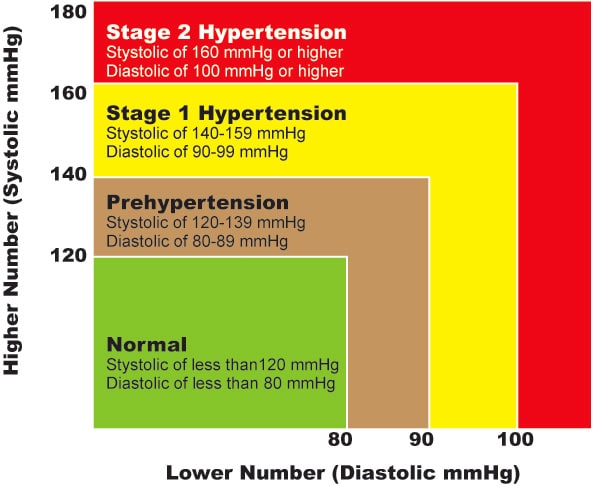
These broad classifications are primarily designed for the purposes of standardizing our classification of hypertension. This is helpful for the purposes of standardizing research and treatment protocols.
Severely elevated blood pressures (serial measurements over several hours) consisting of systolic blood pressures greater than 180 mmHg and diastolic blood pressures greater than 120 mmHg that are associated with symptoms of severe headache, chest pain, dizziness, or shortness of breath is considered to be a hypertensive urgency or emergency. This condition should be evaluated and treated immediately.
Heart attack is the vernacular phrase for what is medically known as a myocardial infarction. The mechanism is usually a condition when there is a sudden loss of blood flow to a section of the heart muscle with associated heart muscle death. The usual mechanism is the sudden occlusion of a blood vessel due to the rupture of a vascular plaque.
The typical symptoms that individuals experience are substernal chest discomfort, shortness of breath, nausea with or without vomiting, sweatiness, or fatigue. Often, individuals will either have very mild symptoms or no symptoms at all. This is referred to as a “silent heart attack.” Individuals with a history of a heart attack are at risk for having a recurrent heart attack.
The usual underlying condition is coronary artery disease. This is a condition in which there is inflammation and plaque development in the walls of the coronary arteries. The coronary artery vasculature is a site of ongoing oxidative stress and accelerated inflammation. This adverse biochemical process could also involve other cardiac structures such as the heart valves and muscle tissue. Hence coronary artery disease is often associated with valvular disease and primary heart muscle dysfunction.
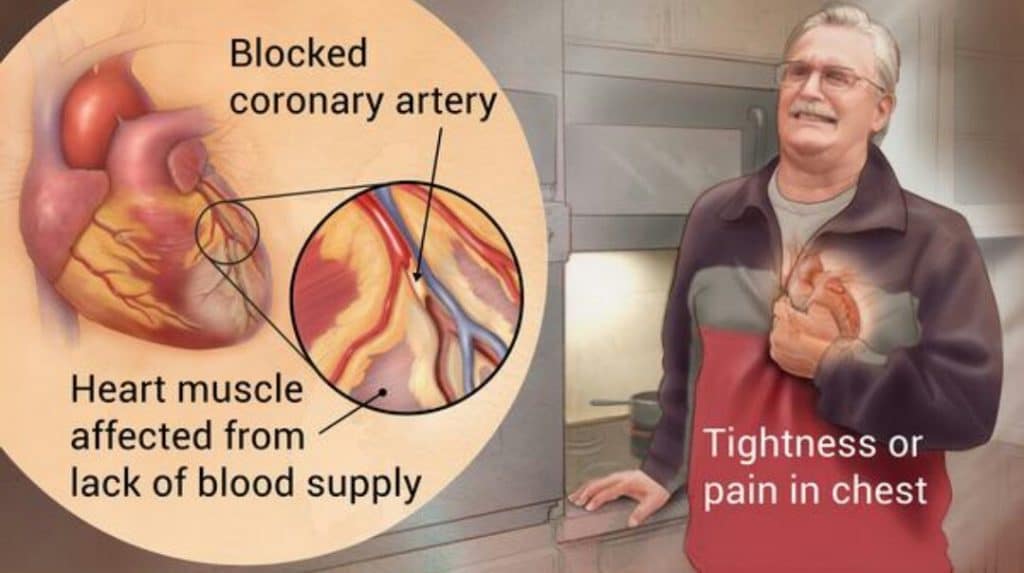
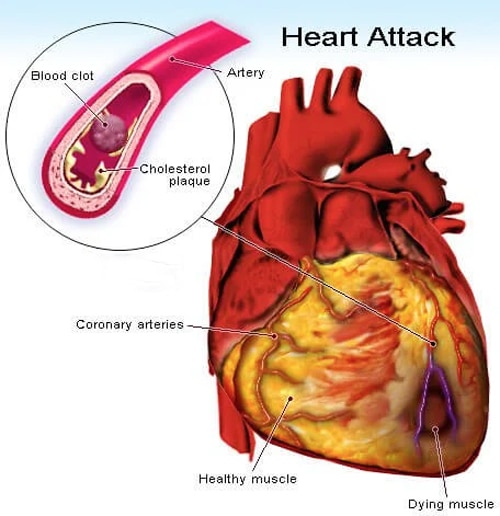
The coronary blood vessels with underlying inflammation and oxidative stress is subjected to periodic, episodic flare-ups with one or more types of triggers. Examples of triggers include infections (bacterial, viral, or other), emotional stress such as anger, surgery, or eating a very unhealthy meal (one with lots of grease and fat), to name a few. The common aspect of these triggers is their potential to cause a sudden, large increase in inflammation. This is like having a “cytokine storm” localized to the blood vessel. Such triggers can lead to a sudden vascular closure resulting in a heart attack as described above. Other types of clinical conditions that are associated with heart attacks include heart failure, valvular dysfunction and more.
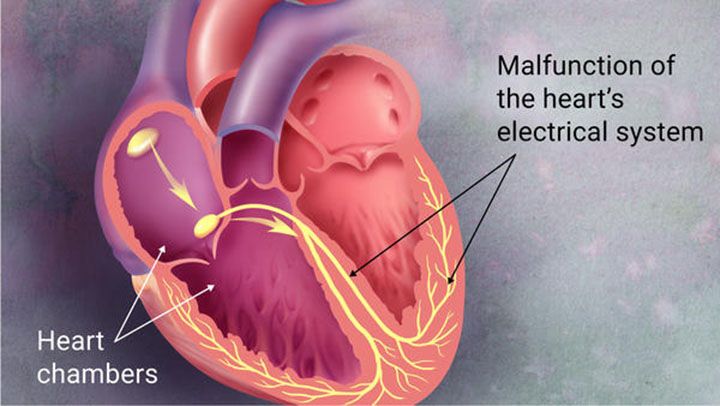
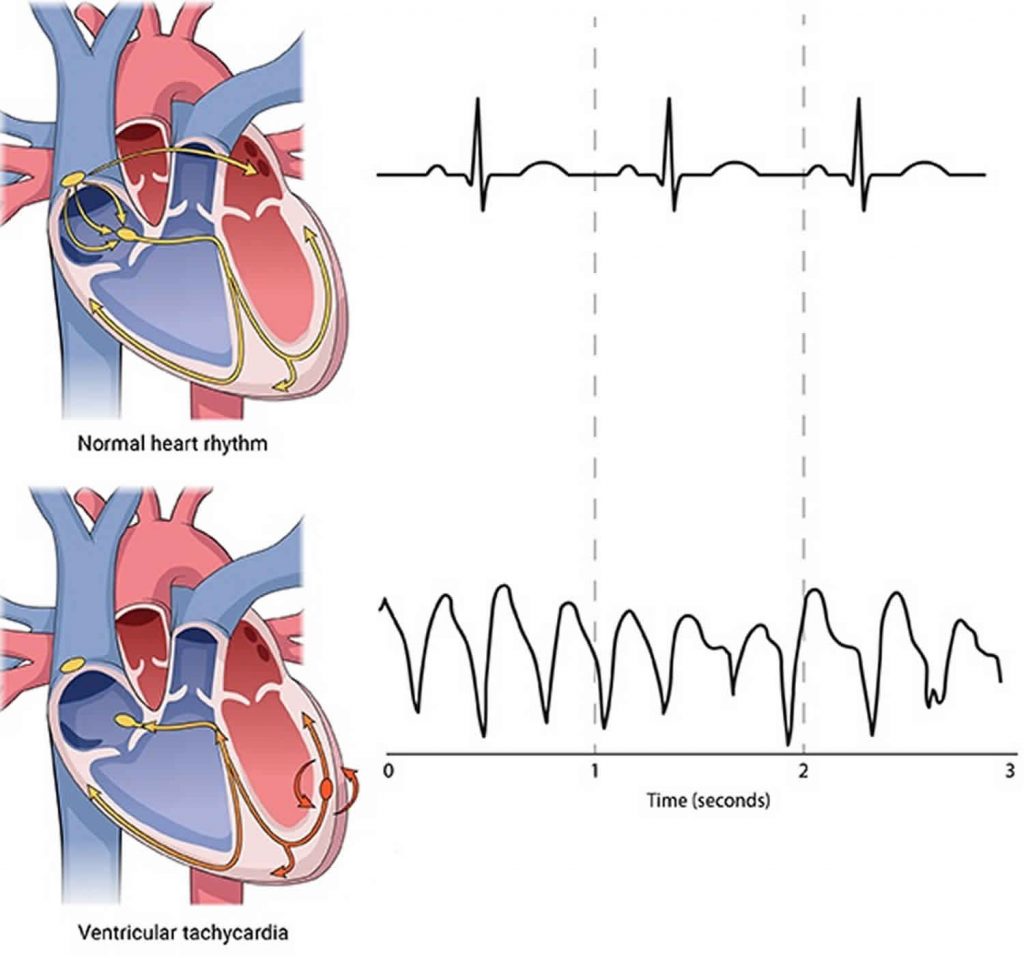
Cardiac arrhythmia is essentially when the heart is “without” normal rhythm or “off” rhythm. The normal rhythm of the heart consists of when an electrical signal initiates in the native pacemaker called the sinus node. This “native pacemaker” sends electrical signals through the heart at a certain rate (based on the body’s needs) in a specified conduction order. The electrical signal initially passes through the special electrical pathways of both upper chambers (the atria), then through a special filter that connects the upper and lower chambers (the atrioventricular node or AV node) and then through special electrical pathways in both lower chambers.
Arrhythmias are usually classified based on whether they originate in one of the upper chambers (atrial arrhythmias) or one of the lower chambers (ventricular arrhythmias) of the heart. While the detailed mechanisms of different arrhythmias is beyond the scope of this discussion, it is important to understand that they are generally due to structural abnormalities of the heart, metabolic abnormalities, or neurological abnormalities (usually from the central nervous system).
These underlying mechanisms for cardiac arrhythmias are subject to the same biochemical disorders of chronic diseases (inflammation and oxidative stress). Additionally, other forms of heart disease can contribute to cardiac arrhythmias through structural damage to the heart (heart attack) or metabolic changes within the heart (hypertension, diabetes).
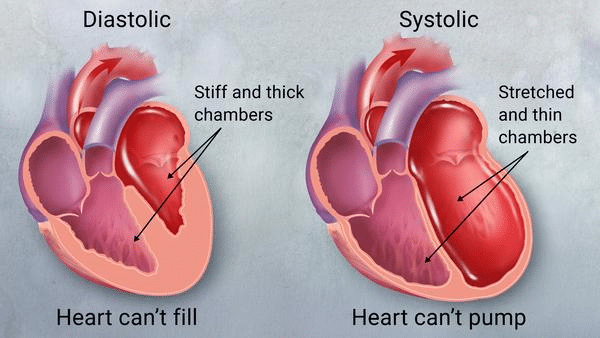
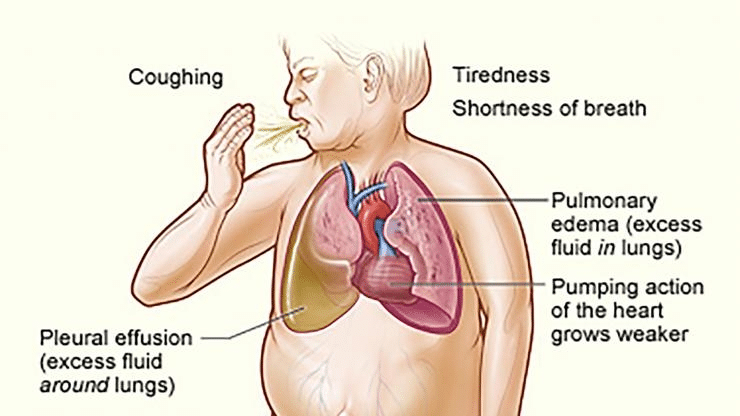
Heart failure is a clinical syndrome associated with the heart’s inability to circulate blood commiserate to the body’s physiologic needs. Generally, this is due to insufficient blood flow due to poor emptying, or poor filling of the left lower chamber of the heart (left ventricle), or both. Symptoms of heart failure are vast and may not appear to be related to heart disease. This is due to the fact that all parts of the body requires blood flow and hence impaired blood flow can lead to symptoms in organs remote from the heart. Therefore, while symptoms such as chest discomfort or shortness of breath are usually reported, loss of appetite, fatigue, mental dysfunction, or weakness in the extremities can also be seen.
There are many causes of heart failure. Most are due to other underlying heart diseases such as coronary artery disease causing ischemia (poor blood flow and oxygen supply to the heart muscle) or heart attack, high blood pressure, heart valvular disease, or chronic arrhythmias. Chronic systemic illnesses can also contribute to heart failure. Systemic conditions commonly associated with heart failure include diabetes, systemic autoimmune diseases like Lupus, anemias, or certain cancers. A significant number of patients presenting with heart failure will have no easily identifiable cause and hence referred as having idiopathic heart failure. These causes of heart failure are likely due to underlying metabolic abnormalities such as mitochondrial dysfunction or other cellular dysfunctions or biochemical deficiencies (deficiencies of CoQ10, glutathione, magnesium, vitamin C, or more).
Syncope is a condition that is due to a transient loss of consciousness (temporarily passing out). It can be due to many different causes. Unless the syncopal episode results in physical injury, the underlying cause of syncope is usually the most important factor relating to the individual’s overall prognosis.
Generally, we classify syncope as cardiac (related to heart disease) or non-cardiac (other causes). The prognosis is generally worse if the syncope is due to heart disease. Hence, individuals with a known history of heart disease and syncope, should be evaluated by a cardiologist immediately. Cardiac causes include heart attack, arrhythmia, or low blood pressure. Non-cardiac causes include an abnormal loss of blood vessel tone with or without a decrease in heart rate secondary to an autonomic central nervous system dysfunction, anemia, dehydration, medications, and more.
In general, effective treatment of syncope involves the treatment of the underlying health condition.
Circulatory diseases in general consist of the dysfunction of blood vessels (veins and arteries) throughout the body. The circulatory system consists of three major types of vascular structures: arteries, veins, and lymphatics. The simplest description of these structures is that they are tubular structures analogous to pipes that channel oxygen and nutrients towards organs and tissues and carbon dioxide and waist away from them. This analogy is an oversimplification because these vascular structures are dynamic functioning organs in an of themselves. A detailed review of this category is beyond the scope of this discussion. However, we will briefly review two major types of circulatory disease below.
Cerebrovascular
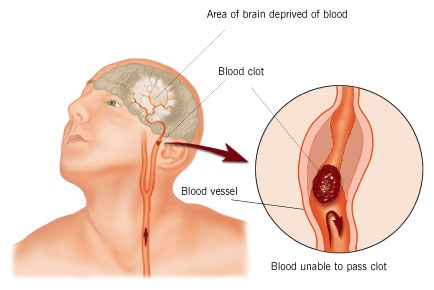
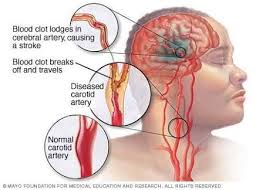
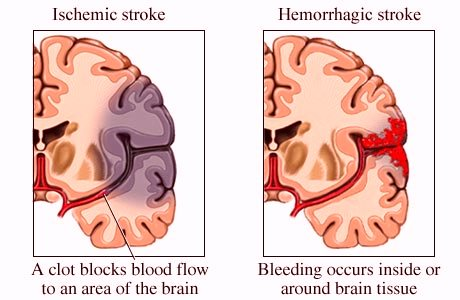
Cerebrovascular disease consists of abnormalities of vascular structures of the brain. More specifically the arterial flow to the brain. Similar to coronary artery disease, these vessels can develop inflammation in their walls resulting in fibrosis, calcium buildup and plaque formation. Breakdown in the linings of the vascular walls can lead to the formation of ballooning out of the walls known as aneurysms.
The clinical manifestations include stroke (sudden loss of blood flow to a section of the brain), transient ischemic attack (mini stroke due to temporary loss of blood flow to a section of the brain), memory loss, dementia, and nonspecific symptoms such as brain fog. Symptoms associated with stroke often are related to neuromuscular dysfunction such as weakness and numbness. Other stroke related symptoms consist of speech impairments, loss of balance, and loss of taste and smell on rare occasions.
It is important to note here that a significant number of strokes are related to an abnormal heart rhythm known as atrial fibrillation. The mechanism here is in part due to the possible embolization (release from the heart to the brain) of a blood clot to a branch of a blood vessel in the brain resulting brain tissue death. This embolization mechanism likely requires the presence of associated vascular abnormalities.
Peripheral Vascular
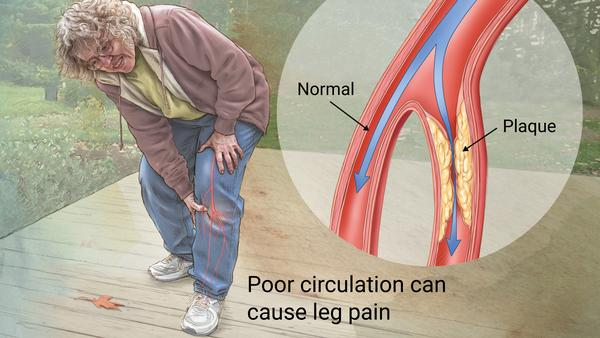
Peripheral vascular disease is also a blood vessel disorder similar to coronary artery disease and cerebrovascular disease. In fact, individuals with any of these disorders likely have vascular disease of the other types to varying degrees. Clinical manifestations of peripheral vascular disease most commonly involve the lower extremities (legs) to a much greater degree than the upper extremities (arms). The likely reason for this difference is the increased metabolic demand on the lower extremities due to their weight-bearing responsibilities.
Examples of clinical manifestations include discomfort in the legs associated with walking or other physical exertion. Numbness and tingling are usually due to neurologic abnormalities; however, individuals with significant peripheral vascular disease frequently have these symptoms also. Poorly healing wounds such as ulcers and abrasions could be signs of peripheral vascular disease due to poor circulation and delivery of blood, oxygen, and nutrients. Loss of hair in the lower extremities can be an early sign of peripheral vascular disease.
Acute obstruction of the peripheral blood vessels can cause a sudden loss of blood flow to an extremity resulting in sudden loss of oxygen to that tissue bed and death to the area. Such conditions would require emergency restoration of blood flow to avoid loss of limb.
Optimize your health with weekly access to health tips, recipes, clinical case studies, and expert panel live streams.
I understand that I am signing up for the Garden Kitchen Program. All meal plans are non-refundable. Prices are subject to change. For discounts and other promotions, please see a wellness coordinator for more details.
Any changes or cancellations to meal plan and pick up schedule requires at least 48 hours’ notice and must be communicated via email at mealplans@montgomeryheart.com . Customers may receive credit to the Garden Kitchen for the remaining balance on a meal plan. If meal plan items are not picked up on the scheduled date with no notice, the items will not be replaced and will be counted against your remaining days.
Our store offers products with peanuts, tree nuts, soy, nut milks, and gluten.
All meal plan sales are final. No substitutions or other alterations are allowed. No refunds are allowed for missed pick-ups. No substitutions are allowed on meal plans A-E.
All meal plan orders placed by the end of day Friday will begin on the Tuesday the following week. Pick up times are on Tuesdays and Fridays, between 1 pm and 6 pm. Deliveries will be scheduled to arrive on Tuesdays and Fridays.